Proposed changes could make weight-loss drugs more accessible to millions of Americans
CMS proposes changes to Medicare and Medicaid to cover weight-loss drugs, recognizing obesity as a disease. This could expand access to millions, sparking debate over costs and benefits.
The U.S. Centers for Medicare and Medicaid Services (CMS) on Tuesday, Nov. 26, announced proposed changes in Medicare and Medicaid that would formally recognize obesity as a disease, meaning weight-loss drugs would be covered as a Part D drug if approved by the Trump administration.
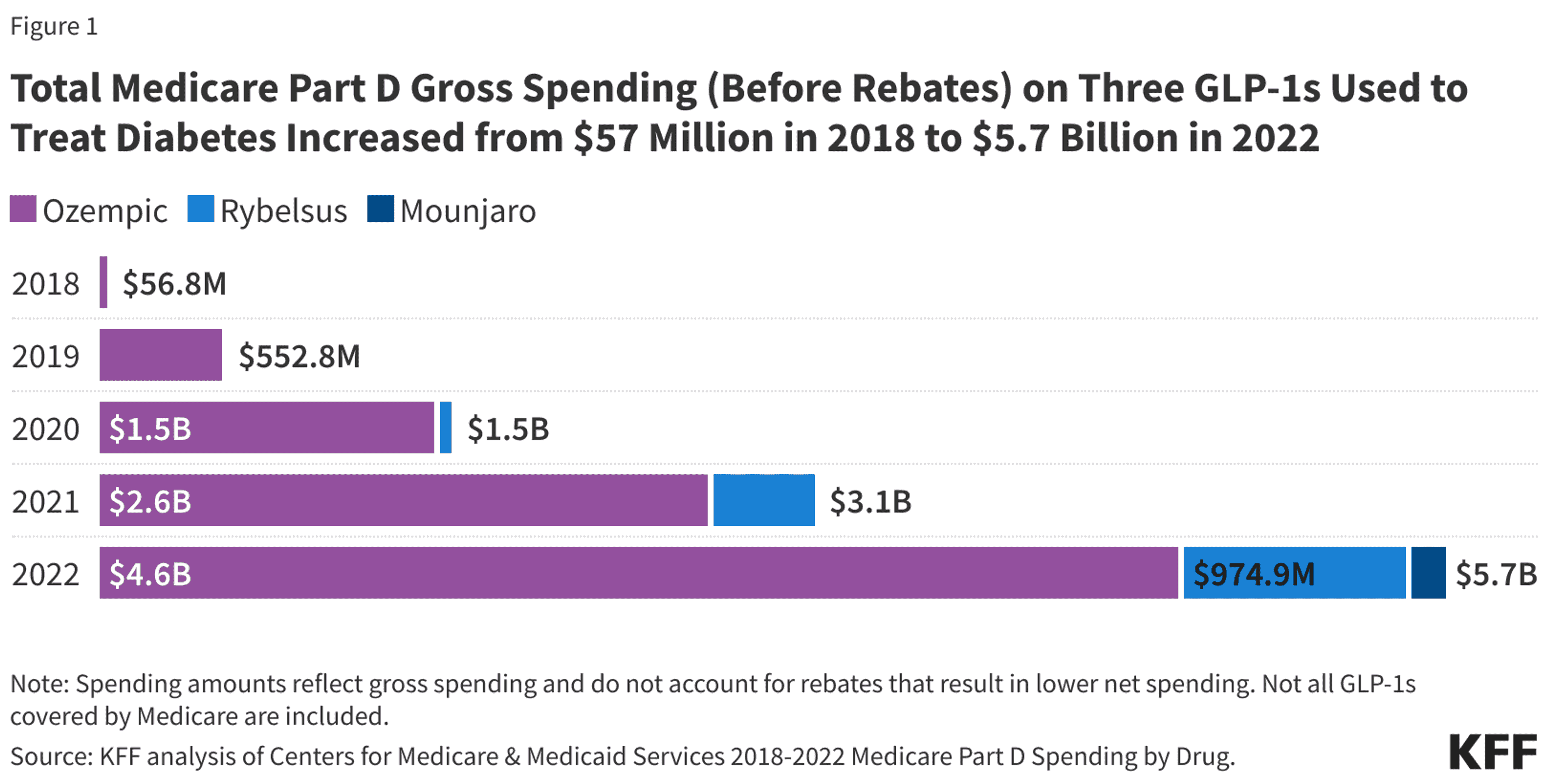
Previously, weight loss drugs such as Ozempic, Wegovy, Novo Nordisk, Mounjaro and Zepbound, were covered by Medicare Part D only if the drug was being used to treat another condition that was medically accepted, such as Type 2 diabetes or to reduce the risk of major adverse cardiovascular events with patients who had heart disease.
“CMS’ revised interpretation would recognize obesity to be a chronic disease based on changes in medical consensus,” the CMS stated in a fact sheet on its website. “However, CMS would not consider that interpretation to extend to individuals who are overweight but do not have obesity as ‘overweight’ is not considered a disease. Therefore, we would continue to exclude anti-obesity medications from Part D coverage when being used in individuals who are overweight but without obesity or another condition that is a medically accepted indication.”
The proposal requires a 60-day public comment period before it can go into effect, leaving it up to the incoming Trump administration whether to enact the change.
The weight-loss drugs are injected weekly and mimic a hormone called GLP-1 (for Glucagon-like peptide), which helps control blood sugar, metabolism and helps people feel full. The drugs were approved by the Food and Drug Administration in 2005. Potential side effects include nausea, diarrhea, vomiting, constipation, abdominal pain and dyspepsia.
Roughly 71 million people, or one third of the U.S. adult population were classified as obese in 2021, according to KFF, a not-for-profit health policy and news organization. Obesity is defined by having a body mass index of more than 30%. KFF reported that out-of-pocket costs for the drugs without insurance or Medicare coverage, can be in excess of $1,000 per month. The measure is expected to give access of the drugs to 3.5 million people on Mediccare and 4 million on Medicaid, The Associated Press reported.
The AP also reported that Tuesday’s announcement could set a showdown among conflicting positions with Trump’s future Cabinet members.
A bipartisan coalition of congressional members has lobbied for the drugs to be covered by Medicare, the AP reported. Robert F. Kennedy Jr. — who is President-elect Donald Trump's pick for secretary of Health and Human Services — is an outspoken opponent of the weight-loss drugs, but U.S. Health and Human Services Secretary Xavier Becerra told the AP that Tuesday’s announcement is “a game changer for Americans who can’t afford these drugs otherwise.”
The decision could cost taxpayers as much as $35 billion over the next decade. However, proponents of the move believe the measure could save the government from spending billions treating chronic illness that stem from obesity.
Earlier this year, Kennedy told federal lawmakers that “for half the price of Ozempic, we could purchase regeneratively raised, organig food for every American, three meals a day and a gym membership for every obese American,” he said, according to AP.
Connect with the Southeast Missourian Newsroom:
For corrections to this story or other insights for the editor, click here. To submit a letter to the editor, click here. To learn about the Southeast Missourian’s AI Policy, click here.