The vets' views
POPLAR BLUFF, Mo. -- For Allen Gulley, a veteran returning home after 10 months in Iraq and suffering from incessant ringing in his ears, the two words he didn't expect to hear when he asked for treatment were "prove it." But Gulley, 35, who returned to his hometown of Poplar Bluff and was treated at John J. Pershing Veterans Hospital, says he was told just that by doctors. He's still fighting to have the connection between his hearing loss and combat acknowledged by Veterans Affairs...
POPLAR BLUFF, Mo. -- For Allen Gulley, a veteran returning home after 10 months in Iraq and suffering from incessant ringing in his ears, the two words he didn't expect to hear when he asked for treatment were "prove it."
But Gulley, 35, who returned to his hometown of Poplar Bluff and was treated at John J. Pershing Veterans Hospital, says he was told just that by doctors. He's still fighting to have the connection between his hearing loss and combat acknowledged by Veterans Affairs.
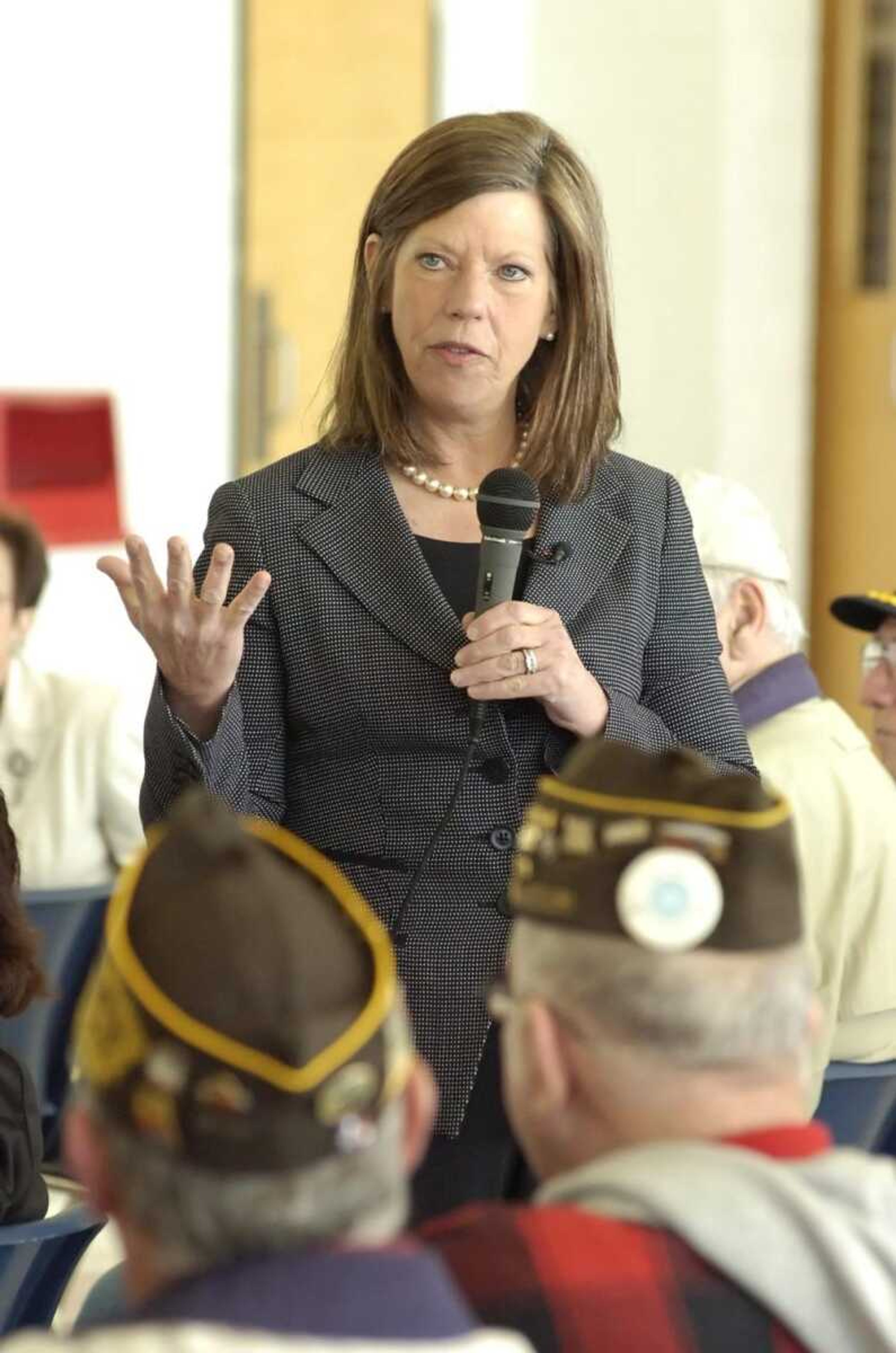
Gulley's problem was one of many discussed Wednesday when Rep. Jo Ann Emerson, R-Cape Girardeau, made an unannounced visit to the VA hospital and afterward held a scheduled discussion with about 35 veterans at the Black River Coliseum.
While most applauded the care they receive at John J. Pershing, they pointed to systematic problems that cause veterans as a group to receive inferior care.
Gulley, a National Guardsman, was deployed to Iraq as a mechanic in 2005. Due to staffing shortages, he was assigned to man the turret gun on an armored Humvee and eventually completed 27 combat missions. In October 2005, while in that position, his convoy hit an improvised explosive device and shrapnel hit his vehicle. Shortly after the incident, Gulley began to experience loud ringing in his ears that he believes to be a chronic condition called tinnitus.
When he returned home later that year, he went to be treated at the VA hospital hoping to receive a "service connection," which amounts to a doctor's acknowledgment that his affliction is service-related and the treatment will be paid for by the VA.
That's when Gulley got a shock.
"They basically said I could not prove it," Gulley said. "They said, and I believe this is the official statement they gave me in the letter, that I couldn't prove I was exposed to anything traumatic enough to cause hearing loss."
Gulley said his doctor asked him whether he could prove he visited a doctor for tinnitus while in Iraq. Gulley said he never saw a doctor because the explosion occurred on the first day of a seven-day mission. He also said a stigma is associated with soldiers asking for help.
Emerson said putting the burden of proof on the soldier is "outrageous" and a restriction that "should be changed."
Proof of trauma
Ray AuBuchon, a veterans service officer with the Missouri Veterans Commission, said Gulley needs to sit down with a service officer and go through an evaluation for his claim to be approved by VA. With proper advocacy, AuBuchon thinks Gulley's case will be approved.
But AuBuchon said the "burden of proof" problem is even harder on soldiers seeking treatment for post-traumatic stress disorder in the VA system.
The VA requires a "stressor" or documented combat incident in order to pay for the PTSD treatment of veterans. AuBuchon said this procedure is outdated in the age of counterinsurgency warfare. Modern warfare, he said, leaves soldiers with frayed nerves after months of being "constantly keyed up."
"They may not see an IED go off, they may not have anybody killed around them, but unlike previous wars, these guys are in 24-7 combat and they're developing PTSD as a result of that alone," he said.
AuBuchon said a PTSD claims takes six to 12 months for the VA to process. The claim typically requires the Department of Defense to verify any "stressor" information.
Emerson also believes this process is outdated.
"The fact that there has to be a particular incident that causes PTSD seems to me not to reflect psychiatric science," she said.
Emerson's staff took information from veterans who needed assistance at the event. Emerson promised to pursue all unsatisfactory VA claims cases.
Communication problems
Another consistent complaint from veterans at John J. Pershing is a difficulty interacting with doctors there. Most doctors at the hospital are foreign-born and difficult to understand, say patients. At times, they say, the doctors do not attempt to listen to their symptoms.
Roger Hubbard, 65, is a former Navy Seabee and a Vietnam veteran. About a year ago, his riding lawn mower fell on him while he was below making repairs. A couple of days later he started spitting up blood and went to the hospital for treatment. He said his foreign-born doctor either did not listen or could not understand him. The doctor took a blood test instead of asking for an X-ray.
"There's a lot of confusion," he said, expressing a sentiment echoed by others who spoke at the coliseum event.
Nancy Arnold, the medical center director at John J. Pershing, said more than 90 percent of the doctors there are foreign-born. Everyone, though, must pass English exams, she said.
"The VA doctors are not paid like physicians in the private sector. We have not been able to recruit and retain American-born physicians," she said. Arnold added that Poplar Bluff's rural location makes it less appealing to American-born doctors.
Emerson said the lack of native-English speaking doctors was her "number one concern" about John J. Pershing.
Emerson said funding is at the root of almost all problems discussed Wednesday. While the VA's 2006 budget was $70.8 billion, a figure, she noted, that has risen from $44 billion in 2000, the cost of health care has also risen.
tgreaney@semissourian.com
335-6611, extension 245
Connect with the Southeast Missourian Newsroom:
For corrections to this story or other insights for the editor, click here. To submit a letter to the editor, click here. To learn about the Southeast Missourian’s AI Policy, click here.