Technology + Health Care: How the industry is changing
Stigma around behavioral health conditions is slowly diminishing as prominent public figures come forward to disclose their personal challenges with depression, addiction, anxiety, bipolar disorder and other common, yet debilitating, mental health conditions. What to expect in the future...
~From access to health care to utilizing AI for diagnosing patients to issues of data ownership, one thing is sure: technology is changing the health care industry. We reached out to health care providers and specialists from the Southeast Missouri region to hear their perspectives on how this is occurring. Here, they share their thoughts.
Growth of awareness of mental health conditions and substance abuse.
__Stigma around behavioral health conditions is slowly diminishing as prominent public figures come forward to disclose their personal challenges with depression, addiction, anxiety, bipolar disorder and other common, yet debilitating, mental health conditions. What to expect in the future.__
"According to a 2006 study by Mathers and Loncar, it is suggested that by the year 2030, depression will be the leading cause of illness globally after HIV/AIDS. Research (SAMSHA 2017 National Survey on Drug Use and Health) also shows there is an increase in mental health prevalence especially in younger individuals, with 25.8% of youth ages 18 to 25 having a mental health diagnosis and 49.5% of youth ages 13 to 18 having a diagnosable mental disorder. There are many cultural trends that contribute to the increase in mental health issues including the prevalence of cyberbullying, over-utilization of technology causing declines in sleep duration and social interaction, and family/social isolation. Research would indicate that individuals diagnosed with a mental health or substance use issues will continue to rise, and there will remain an elevated need for support services to address mental health and substance use. With the stigma of mental health diminishing and an increase in the need for access to services, it builds even more pressure on mental health and substance use providers who are already over-utilized and bursting at the seams. The positive result is with stigma decreasing, it is becoming more acceptable to reach out for help in one's community and through other available options such as technology-based counseling support. With technology-based counseling support, there is often instant access, and it is provided in the comfort of your own home, removing barriers for individuals who may often not come to traditional office-based services. The optimistic long-term outcome of increased access and reduced stigma would be individuals accessing mental health and substance use treatment resources sooner, leading to earlier intervention which can help to reduce the severity of mental illness and addiction."
~-- Janice Ruesler, director of Counseling and Disability Services at Southeast Missouri State University
"Over the past few years, prominent figures in media, politics and entertainment have increasingly discussed the importance of elevating conversations on sound mental health, helping chip away at former stigmas and misconceptions held too long by too many.
This "normalizing" of behavioral health wellness started a cultural shift nearly five years ago at Ferguson Medical Group. Behavioral health professionals worked with clinicians and administrators to include behavioral health questions on the clinic's intake forms. They also collaborated with clinicians to start behavioral health discussions as part of their general patient conversations. The behavioral health providers work closely with clinicians to communicate with patients that feelings, emotions and behaviors are an essential and very "normal" part of a patient's overall well-being.
The team took that conversation one step further by including a behavioral health professional as part of the discussion. Ferguson Medical Group now keeps a behavioral health provider on call when needed for an immediate consult alongside the clinician in the same exam room during the same visit. By working with a nurse, physician assistant or physician -- someone the family knows and trusts -- those discussions can be less intimidating.
This may seem a small step in the process, but this front-end conversation represents putting the patient's needs, schedule and concerns at the forefront. It allows behavioral health to become a natural part of the patient's overall treatment, helps patients avoid any stigma they may associate with a more traditional behavioral health referral and streamlines any follow-up visits. We come to the patient rather than requiring a patient to come to us.
These appointments also help address behavioral components that link to common medical conditions, including obesity, chronic pain, smoking cessation, sleep disorders, difficulty complying with medications/treatments and substance abuse.
The use of electronic medical records has drastically improved the integration of patient care and behavioral health treatment. Saint Francis Healthcare System has a powerful electronic medical record system that allows clinicians to increase continuity of care across disciplines. For example, if a child is diagnosed with autism, providers can immediately begin establishing services for speech therapy, occupational therapy, psychiatry and physical therapy. All providers are involved and aware of the patient's care and progress. With interactive tools such as MyChart, patients can send texts or questions between appointments, reschedule appointments and review treatment notes -- which engages the patient and increases the likelihood of participation in a treatment program.
Improved technologies, better patient engagement and more overall discussions about sound behavioral health will help patients get the treatments they need. This is just the beginning of making a difference in the health and well-being of our patients and their loved ones."
~-- Dr. David Dahlbeck, Psychologist, Ferguson Medical Group, a Saint Francis Healthcare System Medical Partner
---
Big Tech and health care.
__There's a lot of talk about tech companies entering the care delivery space and having a transformative impact on it -- artificial intelligence and machine learning. Although it may take time, eventually how will these innovations impact care?__
"Although the thought of artificial intelligence (AI) technologies making decisions for us about our health care is a little unnerving, the deep learning and analytical algorithms of artificial intelligence have the ability to transform health care. Microsoft, Google and Apple are three of the tech giants that have been making significant inroads in the use of artificial intelligence in health care. Microsoft has been working on a number of health care initiatives, one of which is a partnership with Nuance Communications to develop ambient artificial intelligence (AI) technology that can listen in on the doctor/patient conversation during a visit, automatically generate the patient note and, eventually, make care plan recommendations based upon the data collected. The automatic generation of the majority of the patient note during the patient visit will reduce some of the documentation stresses faced by physicians and allow them to focus more on the patient.
Google has been working on developing a number of machine learning tools that are capable of reaching human-level accuracy. Two areas in which they have made significant progress is ophthalmology and digital pathology. The algorithm Google has developed to examine retinal fundus images for diagnosing diabetic retinopathy has performed comparably to U.S. board-certified ophthalmologists. Google has also been working on algorithms to assist pathologists in detecting breast cancer in lymph node biopsies. Through their research, Google has developed a tool called SMILY that can compare and analyze cropped digitized pathology images from a database of billions of images in a matter of seconds. This technology can assist clinicians in the early detection of abnormalities in tissue samples, such as those preceding a diagnosis of cancer.
Apple is poised to generate a plethora of personal health care data for research purposes with their downloadable voluntary Research app, continued research into powerful sensor development and software development kits such as the ResearchKit and HealthKit. Apple is partnering with leading health and research institutions to use the massive amount of data generated by Apple products to conduct research in areas such as heart health, hearing and women's health studies. For example, through Apple Watch's powerful sensors and the ECG app, users can be alerted to irregularities in heart rate and rhythms. For users who have elected to participate in Apple's research studies, Apple's Noise app can help researchers examine how long-term sound exposure and levels can impact stress, cardiovascular health and hearing over time. Apple is also working on a study to better understand the relationship between female cycles and behaviors and habits on various reproductive health conditions.
Microsoft, Google and Apple have been partnering with leading health care research institutions such as Harvard, the National Institutes of Health, Stanford and The University of Chicago, to name a few, to use technology to advance health care research. AI technologies, such as those being developed by these three companies, have the potential to help clinicians provide better, more prevention-oriented care with a more personalized focus."
~-- Dr. Dana Schwieger, professor of Management Information Systems at Southeast Missouri State University
---
The balance of power between hospital systems and physician groups.
__The roles of each and how technology impacts patient care.__
"Historically, physicians have been independent practitioners, either practicing solo or joining together in a private practice. Very few were employed by hospitals. Hospitals were dependent on the physician for his/her referrals of patients to the hospital for acute care. Primary care physicians (PCPs) provided the majority of care for their patients, admitting patients to a hospital and only consulting a specialist for a procedure or treatment that they could not provide themselves.
Over the past 15 to 20 years, however, the relationship between physician and hospital has grown to be more symbiotic. Hospitals have taken a more active role in patient management by forming care teams and developing protocols and procedures to help improve outcomes and patient safety. Through this transformation, more and more physicians have given up private practice and chosen employment. Today, roughly 50% of physicians in the United States are now employed by hospitals, thereby forming the nucleus of a health care system.
The patient is now surrounded by a health care team which includes nurses, advance practice professionals, social workers, etc., and is led by a physician directing the care. In the background, the electronic medical record (EMR) provides a platform for communication, order placement, decision support and education, among other things. In this "systemization" of medicine, the EMR provides the connectivity that allows for continuity of care.
The amount of medical knowledge has expanded exponentially over the past several decades, thereby creating more treatment options for any given disease. As a result, fewer problems are managed solely by a primary care physician. With increasing frequency, specialties and sub-specialties that did not exist a decade ago are more involved in patient care. Without a system linking the specialist to the PCP, care would be fragmented. An integrated EMR allows any medical professional involved in the patient's care access to the record. These EMRs frequently have care pathways and protocols for disease entities like asthma that prompt treatment options and provide decision support for any given stage of the disease.
Of course, not all physicians, hospitals or allied professionals are on the same EMR. Health care systems typically employ one EMR across its system, thereby allowing this connectivity and seamless care. Care sought outside of that system is then dependent on the ability of two EMRs to "talk" to one another. While this ability has not yet been fully realized, large EMR companies are working toward the day in which a patient's medical record can be transferred seamlessly between medical professionals and health care systems. In the end, it's not about balancing the power but benefitting the patient."
~-- Dr. Thomas S. Diemer, Chief Medical Officer, Saint Francis Healthcare System
---
Drug pricing and biotechnology.
__How breakthrough innovation from biotechnology and pharmaceutical companies shift focus from the high cost of drugs to finding new and different ways to pay for them in order to expand access to the most innovative products.__
"Drug trends in the United States are shifting from small molecule drugs to medications made using human or animal protein. Medications that fall in this category are defined as biologics -- 32 of the 42 new active substances launched in 2017 were for biologic agents.
While these compounds treat medical conditions that affect a small percent of the population, these also include more common medications like insulins. Biologics are highly specific and treat a disease at the cellular level. Some diseases include multiple sclerosis, rheumatoid arthritis, HIV/AIDS, hepatitis C, cancer, psoriasis and Crohn's disease. These are considered specialty medications and compose 1.9% of the total prescription volume, but account for 37.4% of spending. Also known as "high touch" medications, biologics require thorough counseling for complex medication administration, drug interactions, side effect management and importance of compliance. Biologics offer better patient response and reduce disease progression.
While no generics are available to help reduce cost, some biologics have alternatives called bio-similars. These reduce cost, but practitioners are often apprehensive to switch medications once a patient has proven benefit from brand-specific chemicals.
Biologics come with many barriers. Often the delivery system is complex, such as injections from syringes and pen devices. Biologics are not usually covered by traditional insurance without special authorizations. Once authorized, the co-pays attached to these claims are often unrealistic for patients.
However, there are strategies to help patients gain access. Most of these biologic agents have co-pay cards for privately insured patients which cover the entire cost or reduce it to a minimal fee. Manufacturers will mail a credit/debit card to be used at the register or as an insurance that is entered and billed in the pharmacy computer. Manufacturers' assistance programs cover patients who may not be able to afford specific high-dollar medications. The third avenue of patient cost assistance is through organizations offering grant programs.
At Saint Francis Healthcare System, the Healing Arts and Specialty Pharmacy fills these specialty medications. Manufacturers limit the distribution to pharmacies that offer counseling and the follow-up required for safe administration, a service offered at Saint Francis. Specialty pharmacists initiate prior authorizations, set up patients with co-pay cards, monitor side effects, examine drug interactions, counsel patients on administration of the medications, coordinate home delivery of medications and more."
~-- Katie Bertrand, PharmD, Specialty Pharmacist, Healing Arts and Specialty Pharmacy, Saint Francis Healthcare System
---
How and where health care is delivered.
__How hospitalization cost combined with enabling technologies and evolving patient preferences changes how we think about how and where care is delivered.__
"Nationally, health care and insurance costs are rapidly rising. At Saint Francis Healthcare System, we are going against this trend. In January 2019, we initiated a 15% price decrease.
Some in the health care field might question why Saint Francis is lowering its costs, but with our dedication to delivering exceptional quality and outcomes, we are able to pass our savings on to our patients. Quality costs less -- less time spent in the hospital after surgery, less chance of incurring a surgical site infection and less money spent on prescription medications. It is really that simple. And lowering prices is the right thing to do for our community.
As the largest health care system between St. Louis and Memphis, patients no longer have to travel to receive nationally-recognized care. While there are a few services we do not provide, like treatment for severe burns, organ transplants and some pediatric subspecialties, patients can be confident that the quality of care they receive at Saint Francis is not just acceptable, it is exceptional.
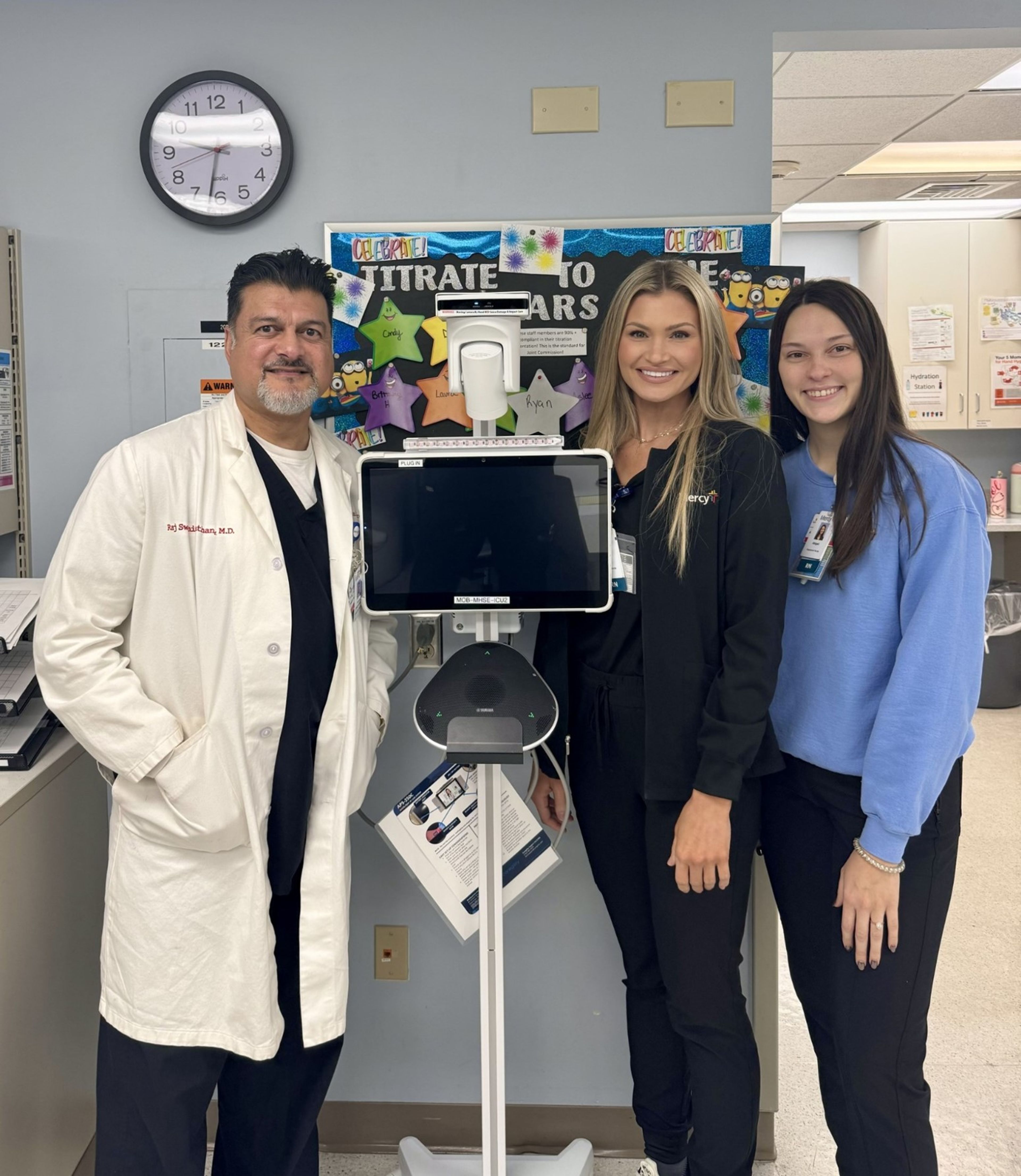
Saint Francis incorporates advancements in technology and training in order to further our efforts to maintain and improve the health of our community. Employing the latest technologies and the very best people allow us to provide comprehensive and effective testing, treatment and services. By continuing to invest in technology and people, we are able to deliver the most advanced, innovative and informed care possible.
At Saint Francis Healthcare System, we are called to serve all who enter our doors with dignity and compassion. Our commitment to quality through the latest technology is just one of the many ways we live our Mission to provide a ministry of healing, wellness, quality and love inspired by our faith in Jesus Christ."
~-- Dr. Maryann Reese, President and Chief Executive Officer, Saint Francis Healthcare System
---
Data privacy, companies that are transparent and ethical.
__Potentially questionable uses and ownership of data will raise eyebrows -- particularly as Americans who have used services for DNA testing come to terms with the fact that they may not have fully understood the privacy implications when they handed their genetic data over for analysis. Who owns the data?__
"In the past, ownership of personal data has been biased toward the company that has the data. There have been legislative efforts in recent years that changed this to favor the consumer. The legislative changes began with the European Union's General Data Protection Regulation (GDPR), which took effect May 25, 2018.
The first point of the GDPR states that "everyone has the right to the protection of personal data." Even though the GDPR was written by the European Union (EU), it applies to all companies that process personal data of citizens of the EU and applies even if that company is based in a non-EU country. As a result, many companies have been forced to change their perspective on who owns the data.
Two key elements of the GDPR is the "right to erasure," also known as "the right to be forgotten," and the "right to restrict processing." These provisions allow individuals to request, either verbally or in writing, a company remove their personal data or how the company uses their data. The company then has 30 days to comply with the request.
While there isn't an equivalent of GDPR in United States federal law even though large U.S. tech companies have advocated for such a law, several states have considered versions of GDPR. In June 2018, California passed a version of GDPR -- California Consumer Privacy Act (CCPA), which goes into effect January 1, 2020. While the CCPA does not include all the provisions of GDPR, it does include some basic protections -- for example, allowing individuals the right to access the data a company has on them. It also requires companies to have a visible footer on websites allowing individuals the ability to opt out of data sharing.
Momentum is clearly on the side of protecting consumers and empowering them with the means to protect their data. As more individuals continue to raise concerns, we will see more legislation driving this change. Even as this continues to change, everyone needs to take the time to review the privacy notices available on websites as these can provide a wealth of guidance on how companies treat data."
~-- Wayne Floyd, CISSP, CPA, MBA, Cyber Security Officer, Saint Francis Healthcare System
---
Role of wearable and other health care devices and their impact on health awareness and care. How do hospitals/doctors view this trend.
__Apple, Google, Amazon, Walmart and more are taking steps to enter the health care market. How do health professionals view these devices and new technology that put health monitoring and management in the hands of patients?__
"At HealthPoint Fitness, we have noticed a trend with our members using apps on their phones that communicate with their smartwatches," says SoutheastHEALTH Fitness Manager Amy Sutherlin, MSA, ACSM, EP-C. "When we remodeled our Cape Girardeau fitness center last year, we intentionally created functional spaces and more open areas within the fitness center to give our members opportunities to use their apps and have space for more functional training opportunities that are shown on many of the apps." Even though the member may be working out "alone" within the facility, there is still a feeling of community that one doesn't receive when working out alone at home, Sutherlin adds.
She also notes that updated bikes in the cycling studio use an app that communicates with members' phones to monitor their work effort in each class. It stores the information in the app so the exerciser can see how they are progressing.
"We also offer Les Mills On Demand programming, which members can access from their homes or on a mobile app at any time," Sutherlin says. "Members can come in and do workouts along with the app, or on days when it isn't possible to come in to the facility, they can stream the programs at home."
HealthPoint's ActivTrax program generates workouts for members so they can follow along to the workout on their phones. Sutherlin says this eliminates the need to walk around with a workout card. "The phone becomes the workout card," she explains.
"All of these apps and advances in technology can enhance members' workouts," Sutherlin adds. "However, even with all of the technology that is available, it's always a good idea to meet with a personal trainer to ensure the workouts people do are appropriate and that they are using proper form. An app can't tell you these things like a one-on-one personal training session can, but combining the technology with support from a personal trainer may result in better adherence to exercise and lifestyle changes."
~-- Sally Owen, SoutheastHEALTH Marketing & Communications Specialist
Connect with the Southeast Missourian Newsroom:
For corrections to this story or other insights for the editor, click here. To submit a letter to the editor, click here. To learn about the Southeast Missourian’s AI Policy, click here.